BACKGROUND:
The introduction of tyrosine kinase inhibitors (TKIs) has significantly improved the long term survival of patients with chronic myeloid leukemia (CML). Patients in cytogenetic remission have life expectancy that approaches that of the general population. The majority of patients with CML remain on TKIs indefinitely. It is unclear whether prolonged exposure to TKIs increases the risk of second malignant neoplasms (SMN) and if malignancies developing in CML survivors harbor similar prognosis to malignancies in non-CML patients.
METHODS:
We utilized the Surveillance, Epidemiology and End Results 18 (SEER 18) registries to evaluate SMN in adult patients diagnosed with BCR-ABL1 positive CML as first malignant neoplasm between 2001 (introduction of TKIs) and 2014(most recent year with available data). Follow up is current to the end of 2014 (November 2016 submission). Using the multiple primary standardized incidence ratio (SIR) session of the SEER*stat software (version 8.1.5), we calculated the SIR of SMNs for CML survivors. Cases diagnosed at autopsy and by death certificate only were excluded. SMN was defined as a metachronous non-leukemia malignancy that developed at least 6 months after the diagnosis of CML. Survival rates for the most common malignancies in CML survivors were compared with tumor site, age, gender, race/ethnicity, histology, grade and stage-matched cases developing in individuals without a prior diagnosis of CML.
RESULTS:
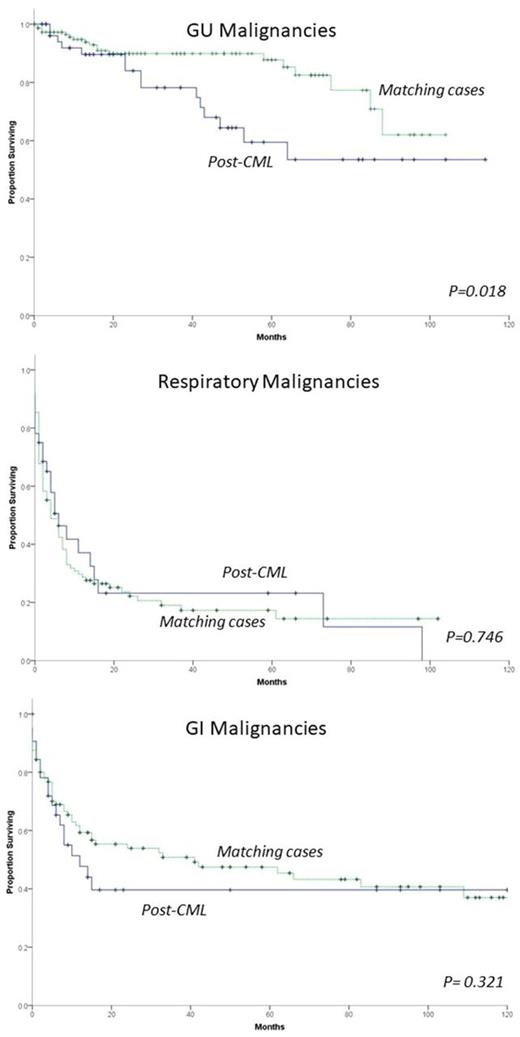
There were 3,407 patients included in the analysis with a median follow up of 41 months. The median age at diagnoses was 53 years (range 20-98) and 56% were men. Of these patients, 170 (4.99%) developed a SMN after a median of 36.5 months from diagnosis of CML (range 6-160) with a SIR of 1.40 (95%C.I. 1.19-1.62) and excess risk of 34.92 per 10,000 persons* year. The most commonly occurring SMNs were lung (n=30), prostate (n=28) and colorectal (n=19). A significantly increased risk was noted for cancers of the respiratory tract (n=32, SIR 1.69, 95%C.I. 1.15-2.4), genitourinary (GU) tract (n=54, SIR 1.39, 95%C.I. 1.04-1.81) and skin excluding basal cell and squamous cell carcinoma (n=13, SIR 1.94, 95%C.I. 1.04-3.32). There was no significant increase in risk of gastrointestinal (GI) tract (n=32, SIR 1.36, 95%C.I. 0.93-1.92), head and neck (n=5, SIR 1.51, 95%C.I. 0.49-3.52) and breast cancer (n=13, SIR 0.85, 95%C.I. 0.45-1.46). Using 3:1 matching (3 de novo malignancies to 1 post-CML SMN case), we compared survival data for cancers of the respiratory, GU and GI tract. Patients with GU malignancies developing after CML had worse overall survival than matched patients without prior CML diagnosis (P=0.018). There was no survival difference between post-CML and non-post-CML patients with respiratory or GI malignancies (Figure).
CONCLUSION:
CML survivors have an increased risk of developing subsequent malignancies as compared to the general population. The increase in risk is more evident for GU, respiratory and non-basal cell, non-squamous cell carcinoma skin cancer. GU malignancies in CML survivors have worse outcomes than in non-CML patients. Future investigation should focus on the biologic mechanism of increased susceptibility of CML survivors to solid tumors.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.